Noninvasive Imaging Technique Devised to Map Electrical Activation of the Heart Directly
By MedImaging International staff writers
Posted on 06 Jun 2011
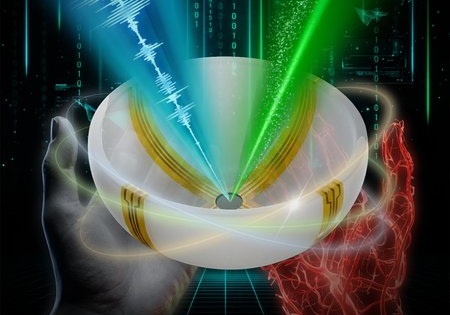
Abnormalities in cardiac conduction, the rate at which the heart conducts electrical impulses to contract and relax, are a major cause of death and disability worldwide. Researchers have been developing a new method, called electromechanical wave imaging (EWI) that is the first noninvasive technique to map the electrical activation of the heart. Based on ultrasound imaging, EWI will enable clinicians to treat arrhythmias more effectively and precisely. Posted on 06 Jun 2011
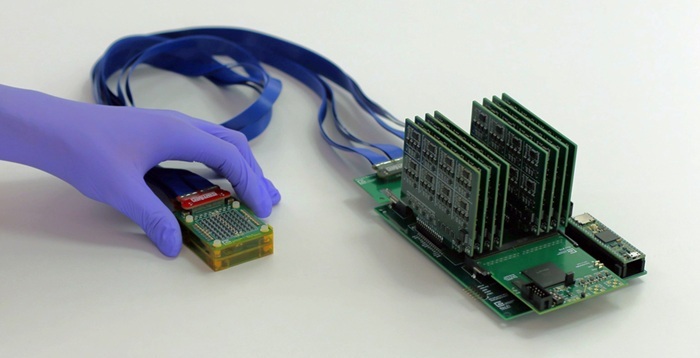
The study's findings were published online in the May 9, 2011, in the journal Proceedings of the [US] National Academy of Sciences. Up until now, other research groups have mostly focused on measuring the electrical activation directly but invasively, through electrode contact, or noninvasively but indirectly, through complex mathematical modeling based on remote measurements. "This is an important breakthrough," said Dr. Elisa Konofagou, who led the research, and is an associate professor of biomedical engineering and radiology at Columbia University's Fu Foundation School of Engineering and Applied Science (New York, NY, USA). "The approach we have chosen--to look at the minute deformations following the electrical activation of the heart--is both direct and noninvasive. Electromechanical Wave Imaging is also eminently translational as it can be incorporated into most ultrasound scanners already available in hospitals and clinics, and can be modified at little or no cost to use our technology."
Using their EWI method, the Columbia engineering team imaged the heart with ultrasound five times faster than standard echocardiography and mapped the local deformations of the heart with their images. The researchers then looked at small regions of the heart (just a few millimeters squared) and measured how much these regions were stretched or compressed every 0.002 seconds. This enabled them to precisely identify at what time each region of the heart began to contract (the electromechanical activation) in all four chambers of the heart. They compared their maps with the electrical activation sequence and found they were closely correlated, at both the natural rhythm of the heart and when the heart was artificially paced.
Arrhythmias occur when the normal electrical activation sequence in the heart is disrupted and their prevalence is expected to rise, as people live longer. In some instances, effective treatments exist. For example, a pacemaker can be surgically placed or a catheter can be brought into the cardiac chambers and used to burn diseased regions of the heart or pacing leads can be implanted in the heart to bypass the diseased conduction system and replace it by artificial electrical activation. However, clinicians cannot always tell where to ablate with a catheter or who will benefit from artificial electrical activation. EWI could help determine in advance which patients can benefit from these treatments or identify with more precision which regions of the heart should be ablated. It could also be used to adapt treatment parameters as the patient's condition evolves.
"Since ultrasound is so safe, portable, and low cost," added Dr. Konofagou, "we can imagine a future where most physicians can carry a portable ultrasound scanner the size of an iPhone and easily get a map of the activation of the heart during a routine visit." Her team has already begun to image patients with arrhythmias and compare their measurements with the gold standard of catheterization and noncontact electrode measurements. If this study is conclusive, they will then move to a larger clinical study.
Related Links:
Columbia University's Fu Foundation School of Engineering and Applied Science