Biodegradable Balloon to Revolutionize Rectal Protection from Toxicity during Prostate Cancer Radiation Therapy
Posted on 30 Aug 2023
Prostate cancer stands as the most common non-skin cancer detected in men and ranks as the second leading cause of male cancer-related deaths, following lung cancer. With a prevalence of 1 in 9 men receiving a prostate cancer diagnosis during their lifetime, over 1.4 million men are globally diagnosed annually. The course of prostate cancer treatment hinges on various factors including cancer growth rate, extent of spread, overall patient health, and potential treatment benefits or side effects. Treatment options like surgery or radiation may be recommended based on evolving test results. However, prostate radiation therapy often leads to a concerning issue – rectal toxicity, a consequence of the close proximity between the prostate and rectum. Despite advanced technology and precise planning, prostate movement during sessions exposes parts of the rectal wall to high radiation doses, resulting in rectal toxicity or proctitis. Hence, there is a strong need for a solution that protects the rectum from the detrimental effects of high-dose radiation. Now, a biodegradable balloon dramatically reduces the chance of rectal toxicity by protecting the adjacent healthy tissues from harmful radiation, thereby minimizing adverse procedural events.
BioProtect Ltd.’s (Tzur Yigal, Israel) BioProtect Balloon Implant System is an implantable, biodegradable balloon that creates a defined, enclosed distance to minimize radiation exposure to the rectum during prostate radiation therapy. Through its distinct design, the new generation balloon achieves up to 18mm separation between the rectal wall and the treatment area prior to initiating radiation therapy. The implantation process involves a minimally invasive, needle-free insertion technique for guiding the balloon using ultrasound with either local or general anesthesia. Once in place between the prostate and rectum, the balloon is filled with sterile saline and positioned to achieve its final, well-defined configuration.
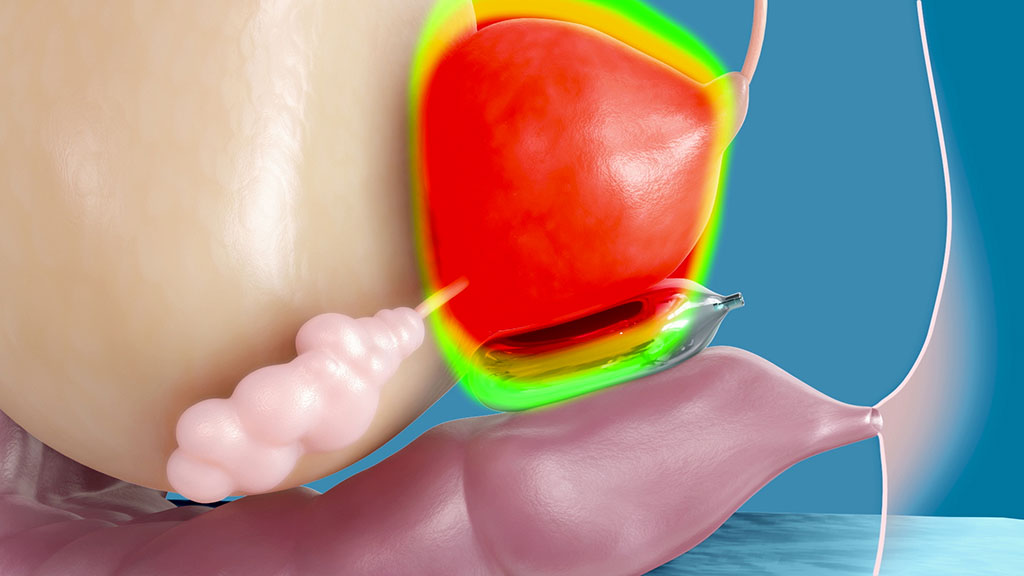
By maintaining a consistent separation between the prostate and rectum, the balloon remains visible across various imaging modalities including CT, MRI, and ultrasound. It forms a protective barrier, allowing for safe radiation therapy. The balloon maintains its size and shape within the body throughout the radiation course, naturally biodegrading over time (typically within six months after implantation), thus negating the need for a separate removal procedure. The BioProtect Balloon Implant System has received clearance from the US FDA.
"We believe that our balloon has the potential to revolutionize rectal protection from toxicity during prostate cancer radiation therapy," said Itay Barnea, CEO of BioProtect. "Not only does it provide better protection to healthy organs, it also supports dose escalation and hypofractionation, which are leading trends in prostate cancer radiation therapy."
Related Links:
BioProtect Ltd.














