AI Outperforms Clinical Tests at Predicting Alzheimer’s Progress from MRI Scans
Posted on 16 Jul 2024
Dementia is a major global health challenge, impacting over 55 million individuals worldwide and costing approximately USD 820 billion annually. Projections indicate that the number of cases will nearly triple in the next 50 years. Alzheimer’s disease is the predominant cause of dementia, responsible for 60-80% of cases. Early detection is pivotal, as this stage is when treatments are most likely to be effective. However, accurate early diagnosis and prognosis often rely on invasive or costly tests such as positron emission tomography (PET) scans or lumbar punctures, which many memory clinics do not have access to. Consequently, up to one-third of patients may receive a misdiagnosis, and others may be diagnosed too late for effective treatment. Now, scientists have developed an AI-based tool that successfully predicts whether individuals showing early signs of dementia will stabilize or progress to Alzheimer’s disease in 80% of cases. This innovation could reduce the need for invasive and expensive diagnostic tests and improve treatment outcomes at an early stage, when lifestyle changes or new medications might be most effective.
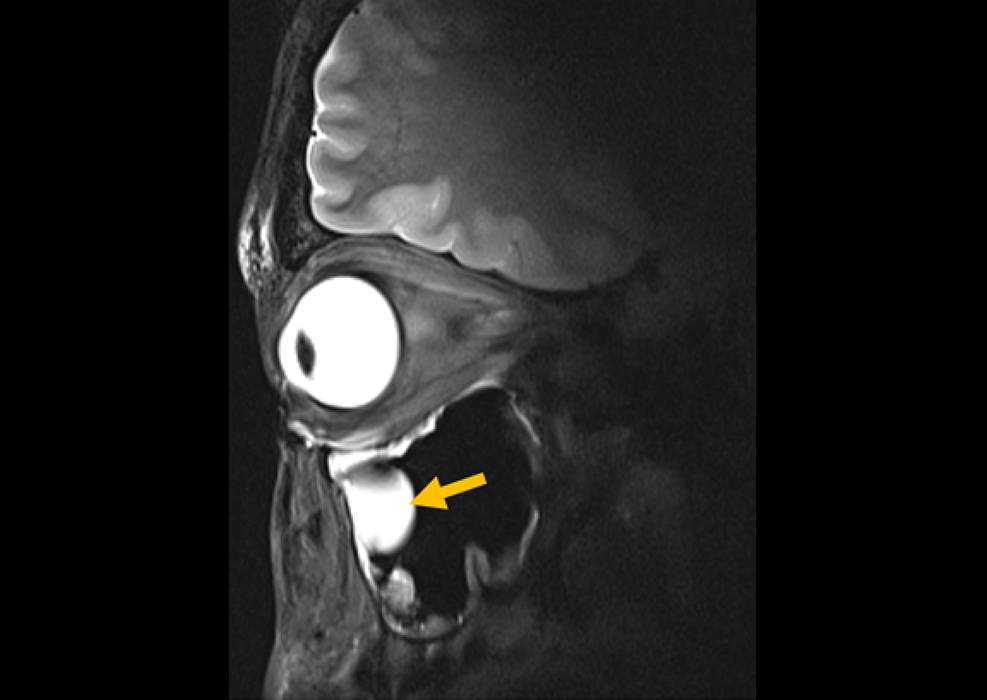
The machine learning model developed by scientists from the Department of Psychology at the University of Cambridge (Cambridge, UK) can predict whether a person with mild memory and thinking issues will develop Alzheimer’s disease, and at what pace. Published in eClinical Medicine, this research has shown that the model surpasses the accuracy of existing clinical diagnostic tools. To develop their model, the researchers utilized routinely collected, non-invasive, and cost-effective patient data—specifically cognitive tests and structural MRI scans depicting grey matter atrophy—from over 400 individuals within a U.S. research cohort. The model was subsequently validated with real-world data from an additional 600 U.S. participants and longitudinal data from 900 individuals from memory clinics in the UK and Singapore.

The algorithm could differentiate between those with stable mild cognitive impairment and those who would develop Alzheimer’s disease within three years. It identified individuals who would develop Alzheimer’s with 82% accuracy and those who would not with 81% accuracy using only cognitive tests and MRI scans. The algorithm was approximately three times more accurate in predicting Alzheimer’s progression than the current standard of care, which relies on standard clinical markers like grey matter atrophy or cognitive scores. This capability significantly reduces the likelihood of misdiagnosis. Additionally, the model enabled researchers to classify individuals with Alzheimer’s at their initial memory clinic visit into three categories: those whose symptoms would remain stable (about 50% of participants), those who would progress slowly (around 35%), and those who would deteriorate rapidly (the remaining 15%).
These predictions were confirmed by follow-up data over six years, highlighting the model's potential to identify individuals at an early stage who could benefit from new treatments and those needing close monitoring due to rapid progression. Importantly, the 50% of individuals with symptoms like memory loss who remained stable could be redirected to alternative clinical pathways, as their symptoms might stem from other causes, such as anxiety or depression. The researchers are now planning to expand their model to other types of dementia, including vascular dementia and frontotemporal dementia, and to incorporate different types of data like blood test markers.
“We’ve created a tool which, despite using only data from cognitive tests and MRI scans, is much more sensitive than current approaches at predicting whether someone will progress from mild symptoms to Alzheimer’s – and if so, whether this progress will be fast or slow,” said senior author Professor Zoe Kourtzi from the Department of Psychology at the University of Cambridge. “This has the potential to significantly improve patient wellbeing, showing us which people need closest care, while removing the anxiety for those patients we predict will remain stable. At a time of intense pressure on healthcare resources, this will also help remove the need for unnecessary invasive and costly diagnostic tests.”
Related Links:
Department of Psychology at University of Cambridge




 Guided Devices.jpg)