Diffusion-Tensor MRI Shows Brain Abnormalities in Patients with Chronic Fatigue
By MedImaging International staff writers
Posted on 12 Nov 2014
Radiology researchers have discovered that the brains of patients with chronic fatigue syndrome (CFS) have reduced white matter and white matter abnormalities in the right hemisphere of the brain. They used neuroimaging techniques to examine the brains of patients with chronic fatigue syndrome and healthy people, and found distinct differences between the two groups.Posted on 12 Nov 2014
Investigators Dr. Michael Zeineh and his colleagues, from by Stanford University School of Medicine (CA, USA), has found clear differences between the brains of patients with chronic fatigue syndrome and those of healthy people.
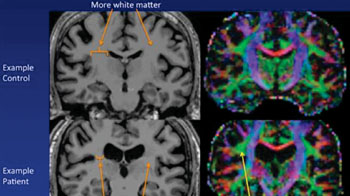
Image: Example of an MR image of a control subject’s brain on top and a chronic fatigue brain on bottom. The ventricles are larger in the chronic fatigue syndrome patient, and there is less white matter. Abnormal microstructure is present on one side in the white matter in chronic fatigue syndrome (Photo courtesy of Michael Zeineh, Stanford University).
The findings could lead to more conclusive diagnoses of the syndrome and may also indicate an underlying mechanism in the disease process. It is not unusual for CFS patients to face several mischaracterizations of their condition, or even suspicions of hypochondria, before receiving a diagnosis of CFS. The abnormalities identified in the study, published October 29, 2014, in the journal Radiology, may help to help solve those ambiguities, according to lead author Michael Zeineh, MD, PhD, assistant professor of radiology. “Using a trio of sophisticated imaging methodologies, we found that CFS patients’ brains diverge from those of healthy subjects in at least three distinct ways,” Dr. Zeineh said.
CFS affects between one million and four million individuals in the United States and millions more worldwide. While all CFS patients share a common symptom—constant fatigue that persists for six months or longer—the additional symptoms can differ from one patient to the next, and they frequently overlap with those of other conditions.
“CFS is one of the greatest scientific and medical challenges of our time,” said the study’s senior author, Jose Montoya, MD, professor of infectious diseases and geographic medicine. “Its symptoms often include not only overwhelming fatigue but also joint and muscle pain, incapacitating headaches, food intolerance, sore throat, enlargement of the lymph nodes, gastrointestinal problems, abnormal blood-pressure and heart-rate events, and hypersensitivity to light, noise, or other sensations.”
The combination of symptoms can devastate a patient’s life for 10, 20, or even 30 years, reported Dr. Montoya, who has been following 200 CFS patients for several years in an effort to identify the syndrome’s underlying mechanisms. He expects that this discovery will hasten the development of more-effective treatments than the currently available ones. “In addition to potentially providing the CFS-specific diagnostic biomarker we’ve been desperately seeking for decades, these findings hold the promise of identifying the area or areas of the brain where the disease has hijacked the central nervous system,” Dr. Montoya said.
“If you don’t understand the disease, you’re throwing darts blindfolded,” said Dr. Zeineh. “We asked ourselves whether brain imaging could turn up something concrete that differs between CFS patients’ and healthy people’s brains. And, interestingly, it did.”
The Stanford investigators compared brain images of 15 CFS patients chosen from the group Montoya has been following to those of 14 age- and sex-matched healthy volunteers with no history of fatigue or other conditions causing symptoms similar to those of CFS. The analysis generated three significant findings, according to the researchers. First, a magnetic resonance imaging (MRI) scan revealed that overall white-matter content of CFS patients’ brains, compared with that of healthy subjects’ brains, was lessened. Gray matter areas specialize in processing data, and the former in conveying the information from one part of the brain to another.
That finding was not completely unexpected, Dr. Zeineh reported. CFS is believed to involve chronic inflammation, possibly as a protracted immunologic response to an as-yet unspecified viral infection. Inflammation is known to inflict damage on white matter. However, a second finding was totally unexpected. Using an advanced MRI technique--diffusion-tensor imaging (DTI), which is particularly suited to evaluating the integrity of white matter--Dr. Zeineh and his colleagues identified a consistent abnormality in a particular part of a nerve tract in the right hemisphere of CFS patients’ brains. This tract, which connects two regions of the brain called the frontal lobe and temporal lobe, is called the right arcuate fasciculus, and in CFS patients it assumed an abnormal appearance.
Furthermore, there was a fairly strong correlation between the degree of abnormality in a CFS patient’s right arcuate fasciculus and the severity of the patient’s condition, as assessed by performance on a standard psychometric test used to evaluate fatigue.
Although the right arcuate fasciculus’s function is still somewhat elusive, its counterpart in the brain’s left hemisphere has been extensively studied. The left arcuate fasciculus connects two critical language areas of the left side of the brain termed Wernicke’s and Broca’s areas, which are gray-matter structures several centimeters apart. These two structures are important to understanding and generating speech, respectively. Right-handed individuals nearly always have language organized in this manner exclusively in the left side of the brain, but the precise side (left or right) and location of speech production and comprehension are not so clear-cut in left-handed people. Therefore, pooling left- and right-handed people’s brain images can be misleading. Furthermore, the finding of an abnormality in the right arcuate fasciculus, pronounced among right-handers, was unclear until the two left-handed patients and four left-handed control subjects’ images were exempted from the analysis. “This study was a start. It shows us where to look.”
Reinforcing these observations was the third finding: a thickening of the gray matter at the two areas of the brain connected by the right arcuate fasciculus in CFS patients, compared with controls. Its correspondence with the observed abnormality in the white matter joining them makes it unlikely that the two were chance findings, according to Dr. Zeineh. Although these results were quite robust, he said, they will need to be confirmed. “This study was a start,” he said. “It shows us where to look.”
The Stanford researchers are in the planning stages of a substantially larger study. The study was supported by GE Healthcare (Chalfont St. Giles, UK) and by the CFS Fund, which is housed in the Stanford.
Related Links:
Stanford University School of Medicine












.jpg)