New System Combines Advanced Optical Imaging with AI Algorithm to Accurately Identify Brain Tumors
By MedImaging International staff writers
Posted on 17 Feb 2020
Researchers from the NYU Grossman School of Medicine (New York, NY, USA) and the University of Michigan (Ann Arbor, MI, USA) have developed a novel method of combining advanced optical imaging with an artificial intelligence (AI) algorithm to produce accurate, real-time intraoperative diagnosis of brain tumors. The imaging technique, stimulated Raman histology (SRH), reveals tumor infiltration in human tissue by collecting scattered laser light, illuminating essential features not typically seen in standard histologic images. The microscopic images are then processed and analyzed with AI, allowing surgeons to see a predicted brain tumor diagnosis in less than three minutes. Using the same technology, after the resection, the surgeons can accurately detect and remove otherwise undetectable tumor.Posted on 17 Feb 2020
The researchers conducted a study to examine the diagnostic accuracy of brain tumor image classification through machine learning, in comparison with the accuracy of pathologist interpretation of conventional histologic images. The results for both methods were comparable: the AI-based diagnosis was 94.6% accurate, as compared with 93.9% for the pathologist-based interpretation.
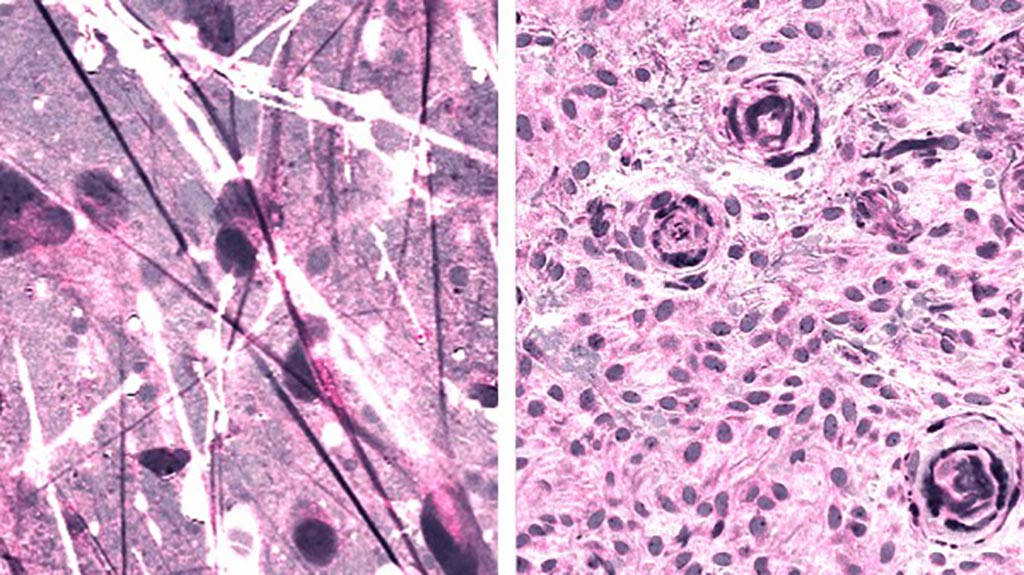
Image: Stimulated Raman histologic images of diffuse astrocytoma (left) and meningioma (right) (Photo courtesy of Daniel Orringer).
To build the AI tool used in the study, the researchers trained a deep convolutional neural network (CNN) with more than 2.5 million samples from 415 patients to classify tissue into 13 histologic categories that represent the most common brain tumors, including malignant glioma, lymphoma, metastatic tumors, and meningioma. In order to validate the CNN, the researchers enrolled 278 patients undergoing brain tumor resection or epilepsy surgery at three university medical centers in the prospective clinical trial. Brain tumor specimens were biopsied from patients, split intraoperatively into sister specimens, and randomly assigned to the control or experimental arm. Specimens routed through the control arm—the current standard practice—were transported to a pathology laboratory and went through specimen processing, slide preparation by technicians, and interpretation by pathologists, a process which takes 20-30 minutes. The experimental arm was performed intraoperatively, from image acquisition and processing to diagnostic prediction via CNN.
Notably, the diagnostic errors in the experimental group were unique from the errors in the control group, suggesting that a pathologist using the novel technique could achieve close to 100% accuracy. The system’s precise diagnostic capacity could also be beneficial to centers that lack access to expert neuropathologists.
“As surgeons, we’re limited to acting on what we can see; this technology allows us to see what would otherwise be invisible, to improve speed and accuracy in the OR, and reduce the risk of misdiagnosis,” said senior author Daniel A. Orringer, MD, associate professor of Neurosurgery at NYU Grossman School of Medicine, who helped develop SRH and co-led the study. “With this imaging technology, cancer operations are safer and more effective than ever before.”
“SRH will revolutionize the field of neuropathology by improving decision-making during surgery and providing expert-level assessment in the hospitals where trained neuropathologists are not available,” said Matija Snuderl, MD, associate professor in the Department of Pathology at NYU Grossman School of Medicine and a co-author of the study.
Related Links:
NYU Grossman School of Medicine
University of Michigan