New 3D Tool Predicts Patients at Higher Risk from Lethal Arrhythmias
By MedImaging International staff writers
Posted on 25 May 2016
Researchers in an interdisciplinary team have developed a non-invasive 3D assessment tool to help clinicians find patients most at risk from lethal arrhythmias, and those who need a defibrillator implant.Posted on 25 May 2016
The proof-of-concept study was published online in the May 10, 2016, issue of the journal Nature Communications. The researchers reported that the new digital technique provided a more accurate assessment of which patients were most at risk, and needed a defibrillator, than current blood pumping measurements.
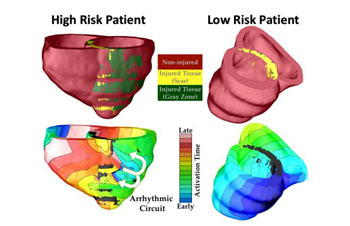
Image: The graphic shows how the VARP 3D computer model was used to classify patients at high risk and low risk for heart arrhythmia (Photo courtesy of Royce Faddis / JHU).
The landmark study was carried out by researchers at the Johns Hopkins University (Baltimore, MD, USA). The researchers used Magnetic Resonance Imaging (MRI) scans and computer-modeling techniques to build a personalized geometrical replica of each patient's heart. The researchers then added representations of the electrical processes, and were able to discover which virtual heart developed an arrhythmia, and which did not. The technique, called Virtual-heart Arrhythmia Risk Predictor (VARP), enabled the researchers to take account of the specific geometry of the heart of each patient, the electrical impulses, and the impact of scar tissue left by a previous heart attack.
The VARP technique was able to predict arrhythmia occurrence in patients four-to-five times better than current ejection fraction techniques, and other non-invasive and invasive clinical risk predictors. The technique was able to eliminate unnecessary implantations of defibrillators, and could also be used to save the lives of a much larger number of at-risk patients.
Professor Natalia Trayanova, Johns Hopkins University, said, "Our virtual heart test significantly outperformed several existing clinical metrics in predicting future arrhythmic events. This non-invasive and personalized virtual heart-risk assessment could help prevent sudden cardiac deaths and allow patients who are not at risk to avoid unnecessary defibrillator implantations. We demonstrated that VARP is better than any other arrhythmia prediction method that is out there. By accurately predicting which patients are at risk of sudden cardiac death, the VARP approach will provide the doctors with a tool to identify those patients who truly need the costly implantable device, and those for whom the device would not provide any life-saving benefits."
Related Links:
Johns Hopkins University














