Diagnostic Algorithm Distinguishes Between Alzheimer’s and Primary Tauopathy Using PET Scans
Posted on 13 Sep 2024
Patients often present at university hospitals with diseases so rare and specific that they are scarcely recognized by physicians in private practice. Primary 4-repeat tauopathies are a notable example. These diseases are primarily associated with movement disorders, but their symptoms can often resemble those of Alzheimer's disease, making precise diagnosis difficult. Now, researchers have found biomarkers that enable doctors to reliably distinguish the two conditions—albeit only with data from a particular imaging technique called positron emission tomography (PET).
In Alzheimer's disease and primary 4-repeat tauopathies, large pathological aggregates of the tau protein are found in the brain. For decades, it has been possible to detect tau proteins for Alzheimer's disease by analyzing the patient's cerebrospinal fluid (CSF). Recently, however, researchers have developed radioactively labeled substances (tracers) that accumulate at the tau aggregates after injection into the body, which are visible on PET images. The new study by researchers at LMU University Hospital (Munich, Germany) shows that tau can be identified with the novel tau PET tracer even in 4-repeat tauopathies—but not in the cerebrospinal fluid, rather in very specific areas of the brain known as the subcortical regions.
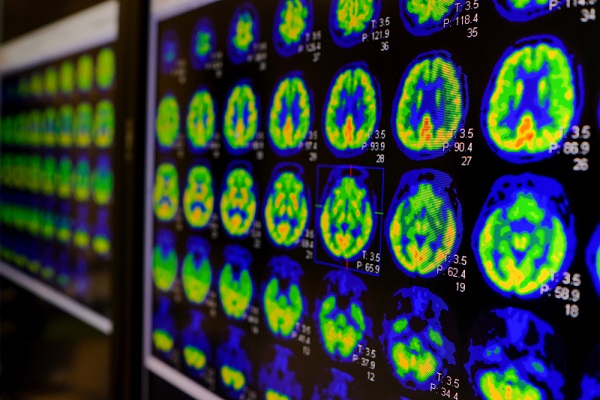
However, the PET signal is just one component of a complex new diagnostic process. The researchers have additionally found new biomarkers that indicate the presence of a 4-repeat tauopathy. Diagnosis becomes highly effective when we analyze a combination of cerebrospinal fluid tests, innovative biomarkers, and PET signals in the subcortical regions. Then, 4-repeat tauopathy can be recognized with a high degree of certainty. The results have been published in the journal Alzheimer's & Dementia 2024.
“The new diagnostic algorithm we developed allows physicians to differentiate with greater precision between Alzheimer’s disease and primary tauopathies, which facilitates earlier and more precise diagnosis and supports personalized treatment strategies,” said principal investigator Professor Matthias Brendel, acting director of the Department of Nuclear Medicine.
Related Links:
LMU University Hospital