Dual-Energy CT Surpasses Pulmonary Function Tests and Conventional CT in Assessing Postoperative Lung Volume
Posted on 03 Nov 2022
Pulmonary function tests (PFTs) and perfusion scintigraphy have limited utility for evaluating postoperative changes in regional pulmonary function after lung cancer resection surgery. Now, new research has found that metrics derived from dual-energy CT (DECT) can provide insight on physiologic changes after lung cancer surgical resection, beyond the information provided by PFTs and conventional CT.
In the study, researchers at the Yonsei University College of Medicine (Seoul, Korea) examined 81 patients (38 men, 43 women; mean age, 60.5 years; lobectomy in 43, limited resection in 38) awaiting lung cancer resection surgery between March 2019 and February 2020. Patients underwent thoracic DECT and PFT evaluation preoperatively and 6 months postoperatively. Pulmonary lobes were segmented, and lobar volume and perfusion ratios - both relative to whole-lung values - were computed. Perfusion measures reflected DECT-derived iodine content. Patients then completed six-month postoperative quality-of-life questionnaires.
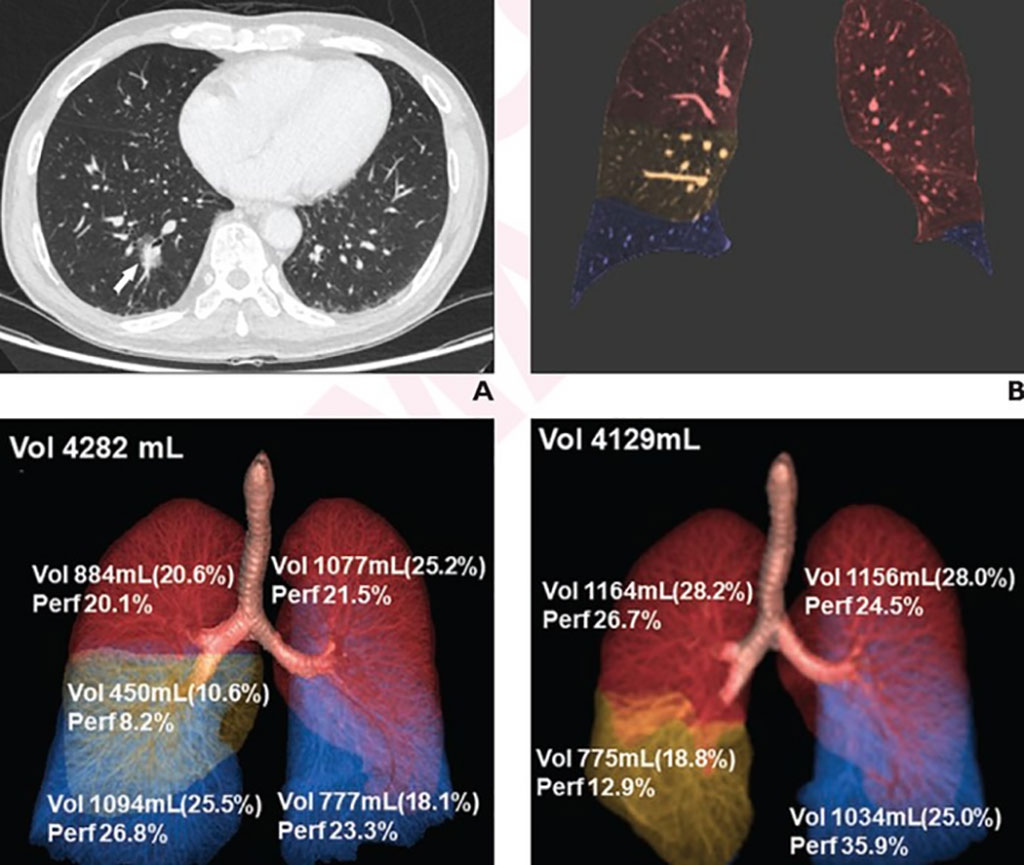
Ultimately, lung perfusion ratio increases were greater after lobectomy than limited resection for ipsi-lateral non-resected lobe(s) (39.9±20.7% vs. 22.8±17.8%) and contra-lateral lung (20.9±9.4% vs. 4.3±5.6%). After right lower lobe lobectomy, the largest postoperative increases in lung volume ratio occurred in the right middle lobe (44.1±21.0%), whereas the largest postoperative increase in lung perfusion ratio occurred in the left lower lobe (53.9±8.6%). Noting some postoperative changes in DECT-derived volume and perfusion parameters showed a correlation with patient-reported postoperative quality-of-life scores, “the findings indicate a potential role of DECT-derived metrics for understanding the variable physiologic impacts of lung cancer resection surgeries,” the authors concluded.
Related Links:
Yonsei University College of Medicine