Combined Digital Screening Detects More Breast Cancers
By MedImaging International staff writers
Posted on 20 Jun 2018
A combination of digital mammography (DM) and digital breast tomosynthesis (DBT) detects 90% more breast cancers than digital mammography alone, according to a new study.Posted on 20 Jun 2018
Researchers at AUSL Reggio Emilia (Italy) conducted a study involving 19,560 women previously participating in the Reggio Emilia screening program. Of these, 9777 women (mean age 56.2 years) were randomly assigned to the DM+DBT arm of the study, and 9,783 women were assigned to the DM arm (mean age 56.3 years). Both arms involved two projections and double reading. Sensitivity, recall rate, and positive predictive value (PPV) at baseline were determined; the ratios of these rates for DBT+DM relative to DM alone were then determined.
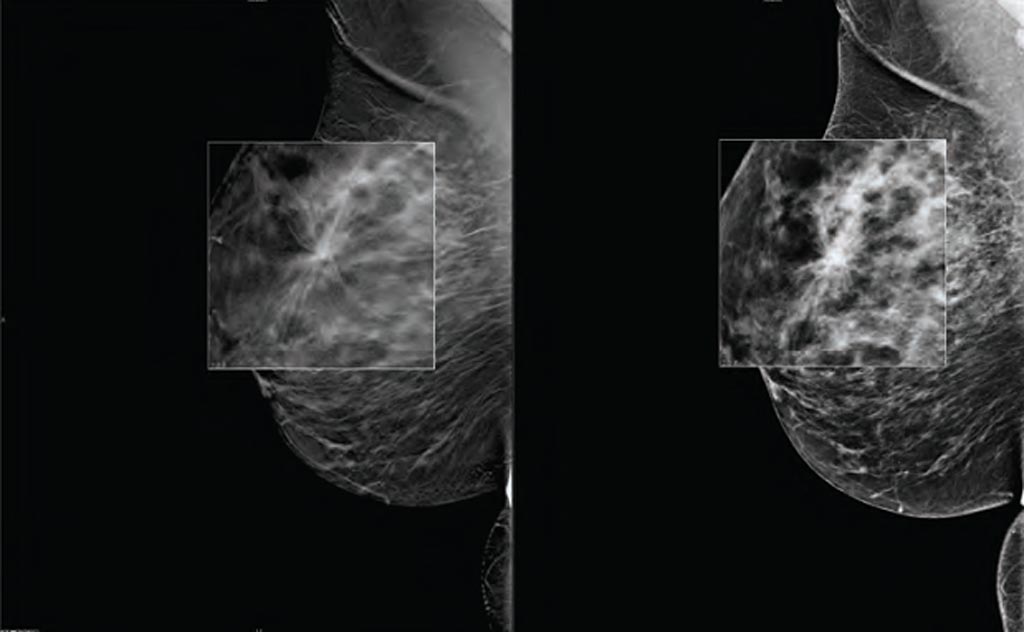
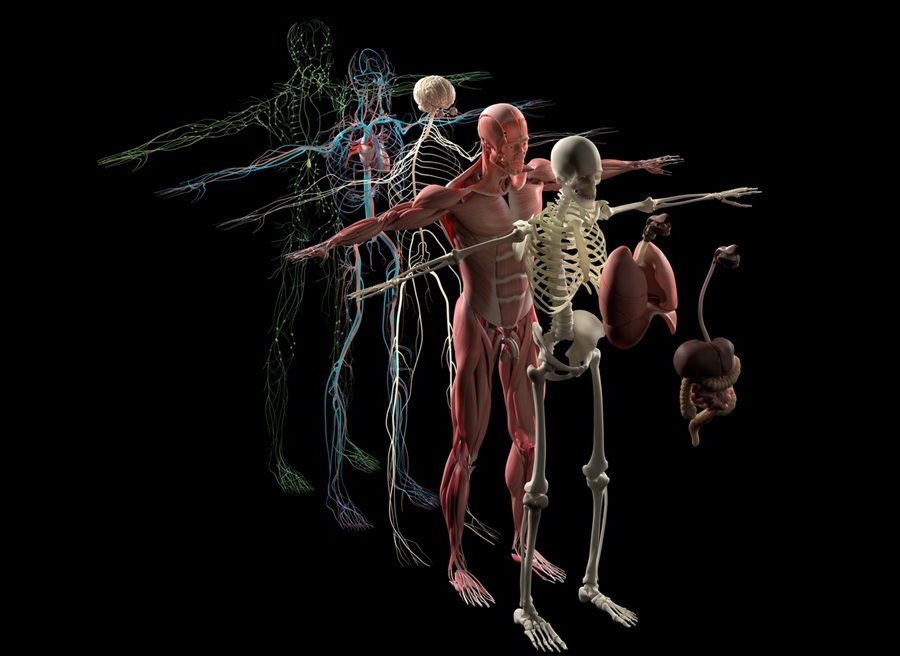
Image: A new study asserts DBT can increase breast cancer detection rates (Photo courtesy of Carestream Health).
The results revealed that the combination of DM and DBT detected 8.6 cancers per 1,000 cases, a rate almost twice that of the 4.5 per 1,000 detected by mammography alone. DBT alone detected 72 of 80 cancers found in the DBT+DM group. The greater detection rate for combined DM and DBT was notable for small and medium invasive cancers, but not for large ones, and was stronger for ductal carcinoma in situ (DCIS). The study was published on June 5, 2018, in Radiology.
“Tomosynthesis and digital mammography is much more sensitive than digital mammography; the vast majority of the advantage is due to tomosynthesis alone,” said lead author radiologist Pierpaolo Pattacini, MD, director of the radiology department. “If these small cancers would never become life-threatening, then we are increasing overdiagnosis and not impacting mortality. Thus, we need to have a measure of the impact of this higher detection rate on the incidence of advanced cancers and interval cancers in the following years.”
“While DBT's higher sensitivity would seem to make it a logical choice for breast cancer screening programs, more research is needed to weigh the benefits of improvements in prognosis and reductions in breast cancer-related mortality from DBT against any undesired effects,” warned study coauthor Paolo Giorgi Rossi, PhD. “The additional reading time DBT would require from breast imagers is another aspect of the technology that requires consideration. For publicly-funded screening programs, this increased reading time would be a big issue, destroying their sustainability.”
DBT mammograms use low dose x-rays to create a three-dimensional (3D) image of the breast, which can then be viewed the in narrow slices, similar to computerized tomography (CT) scans. While in conventional 2D mammography overlapping tissues can mask suspicious areas, 3D images eliminate the overlap, making abnormalities easier to recognize. It is estimated that 3D DBT will replace conventional mammography within ten years.
Related Links:
AUSL Reggio Emilia