CT Trunk Imaging Linked to Higher Nephrectomy Risk
By MedImaging International staff writers
Posted on 15 Jan 2018
People residing in regions with higher rates of abdominal and chest computerized tomography (CT) scan rates face a higher risk of nephrectomy, according to a new study.Posted on 15 Jan 2018
Researchers at Dartmouth College (Hanover, NH, USA) and the Veterans Affairs Outcomes Group (White River Junction, VT, USA) conducted a cross-sectional analysis of Medicare data from 306 hospital referral regions (HRRs) in the United States in order to determine geographic variation of CT imaging referral, and the corresponding association with one of the most consequential sequelae of incidental detection, partial or total nephrectomy.
The study, which included information from 15 million fee-for-service Medicare beneficiaries aged 65-85 years, showed that 43% received either a chest or abdominal CT from January 2010 to December 2014. Risk varied across HRRs, ranging from 31% in Santa Cruz (CA) to 52% in Sun City (AZ). Increased regional CT risk was associated with a higher nephrectomy risk, particularly among HRRs with more than 50,000 beneficiaries. After controlling for adult smoking rates, imaging an additional 1,000 beneficiaries was associated with 4 additional nephrectomies. The study was published on December 26, 2017, in JAMA Internal Medicine.
“Medicare beneficiaries are commonly exposed to CT imaging. Those residing in high-scanning regions face a higher risk of nephrectomy, presumably reflecting the incidental detection of renal masses,” concluded lead author Gilbert Welch, MD, MPH, of Dartmouth University, and colleagues. “We believe surgeons should routinely offer active surveillance for small renal masses, and that patients, after being informed about the small risk of developing metastatic disease, should give the option serious consideration.”
“The results of the study reinforce the need for clinical decision support tools that consider overdiagnosis as harm, as well as the development of consistent standards on how to perform and interpret CT scans,” said Rebecca Smith-Bindman, MD, of the University of California San Francisco (UCSF) in an accompanying commentary. “But that is easier said than done. Once a suspected cancer is found, it is nearly impossible to ignore. The suspected diagnosis opens a Pandora's box, so the only way to decrease overdiagnosis is to avoid unneeded tests in the first place."
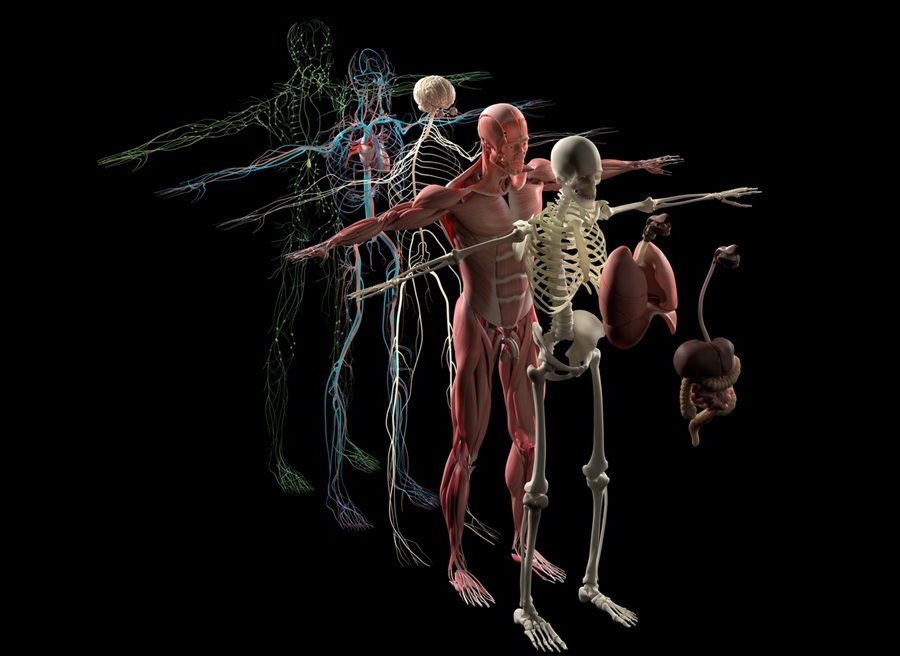
The advent of CT scanning transformed medicine in the early 1970s, enabling clinicians to see details of internal organs that cannot be seen in conventional X-rays. While invaluable in diagnosing the acutely sick and injured, the widespread use of CT scans has an unintended side effect: the identification of what’s known as incidental tumors, unrelated to the clinical symptoms that initiate the test. Such coincidental findings have the potential to lead to overdiagnosis and to overtreatment, including unnecessary surgery.
Related Links:
Dartmouth College
Veterans Affairs Outcomes Group