US MSSP Healthcare Reforms Result in Increased Mammography Screening
By MedImaging International staff writers
Posted on 04 Oct 2016
The US Medicare Shared Savings Program (MSSP) has resulted in an increase in the use of mammography screening in the three years it has run, according to the results of a new study.Posted on 04 Oct 2016
The research was published online, ahead of print, in the October 2016, issue of the journal Radiology. The MSSP program, part of the US Affordable Care Act (ACA), has enabled Healthcare providers, suppliers, and hospitals to participate in, or create, Accountable Care Organizations (ACOs).
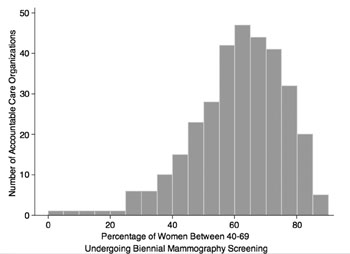
Image: A histogram of screening mammography use in 333 ACOs in 2014 (Photo courtesy of RSNA).
The MSSP program has resulted in small but significant improvements in the utilization of mammography in the participating organizations. The mean increase in screening utilization was 2.6% between 2012 and 2014. Improvements in the utilization of mammography were reported by 61.6% (128) of the 208 ACOs.
ACOs consist of doctors and healthcare providers, such as hospitals, that work together on a voluntarily basis to provide care for Medicare patients. The researchers evaluated mammography screening for women aged between 40 and 69 years, between the years 2012 and 2014, and concluded that further research was needed to understand why some ACOs were more successful than others in their screening programs.
The lead author of the study, Anand Narayan, MD, PhD, from the Johns Hopkins Hospital (Baltimore, MD, USA), said, "The ACA encourages experimentation with alternative-payment models like value-based programs. In the value-based model, instead of being paid for doing more tests and procedures, providers get fixed payments tied to measures of whether they doing a good job or not. Pay-for-performance incentives in ACOs can facilitate collaboration amongst various stakeholders across the healthcare continuum to improve mammography screening utilization and other key population health metrics, results which will become increasingly relevant as imaging reimbursements transition from fee-for-service to alternative or value-based payment. In radiology, we can take an active role in working with other clinicians to ensure that people get appropriate preventive health services. For instance, if a 50-year-old woman comes in for a screening mammogram, we could check to see if she is following screening recommendations for colorectal cancer, cervical cancer and other conditions. While we weren't able to look at specific practices to see what these organizations did, a wide variety of strategies have been discussed. Screening mammography is associated with having access to the health care system. Women start getting screening mammograms and a wide variety of other preventive health services when they start seeing primary care doctors."
Related Links:
Johns Hopkins Hospital