Bimodal Endoscope Detects Early Signs of Esophageal Cancer
By MedImaging International staff writers
Posted on 21 Sep 2016
A near-infrared (NIR) fluorescence and visible light endoscope can aid in the detection of early esophageal malignancy such as in Barrett's esophagus (BE), according to a new study.Posted on 21 Sep 2016
Developed at the University of Cambridge (Cambridge; United Kingdom), the bimodal (NIR and white light) endoscope detects fluorescent wheat germ agglutinin (WGA-IR800CW) dyes in order to construct a clinically translatable image. The endoscope works by co-registering the NIR and white light images, and then removing the honeycomb artifact arising from the fiberoptic bundle. The resulting images provide a field of view of 63o and an image resolution of 182X182 μm.
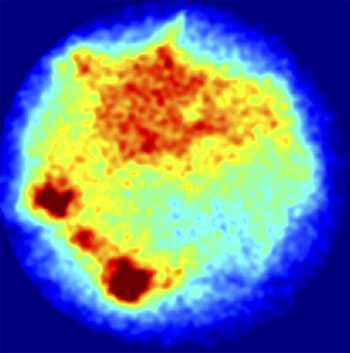
Image: Endoscopic mucosal specimen stained with WGA-IR800CW and imaged with NIR endoscope (Photo courtesy of Sarah Bohndiek).
The researchers successfully demonstrated (ex vivo) that the system can distinguish between gastric and squamous tissue types in mouse stomachs, and accurately detect WGA-IR800CW fluorescence in human esophageal resections. According to the researchers, the new endoscope can moreaccurately delineate dysplasia and help to overcome tissue auto-fluorescence, which limits both sensitivity and contrast of fluorescently labeled lectins under visible light. The study was published on August 4, 2016, in Journal of Biomedical Optics.
“People who are at a high risk of developing esophageal cancer, such as those with Barrett's esophagus, could be closely monitored with this technique, and removing patches of pre-cancerous cells could prevent some cases of esophageal cancer,” said senior author Sarah Bohndiek, PhD, of the Cambridge Cancer Research Institute. “But we need to do some further testing before clinical trials with patients can be set up to see how effective the approach could be at saving lives.”
Barrett’s Esophagus develops as a result of chronic injury from gastroesophageal reflux disease (GERD), which causes metaplasia of the normal squamous epithelium lining of the esophagus, replacing them with goblet cells, which are usually found lower in the gastrointestinal (GI) tract. The significance of BE is its strong association with esophageal adenocarcinoma, a particularly lethal form of cancer.
Related Links:
University of Cambridge