Uncertain Benefit for Imaging After Thyroid Cancer Treatment
By MedImaging International staff writers
Posted on 03 Aug 2016
Researchers at the University of Michigan (Ann Arbor, USA) conducted a surveillance epidemiological study of 28,220 patients diagnosed with differentiated thyroid cancer between 1998 and 2011. The study cohort was followed up to 2013, with a median follow-up of 69 months. Following treatment, 56.7% of the patients had at least one ultrasound, 23.9% had a radioiodine scan, and 14.9% had a positron emission tomography (PET) scan to monitor for signs of cancer recurrence. The main outcome measures were treatment for recurrence of differentiated thyroid cancer and death.Posted on 03 Aug 2016
The results showed that patients who underwent imaging were more likely to undergo further treatment, such as additional neck surgery, additional radioactive iodine treatment, or radiotherapy. The researchers also found that while the use of neck ultrasounds or PET scans did not significantly affect disease-specific survival, radioiodine scans were associated with an improved disease-specific survival. The study was published on July 20, 2016, in BMJ.

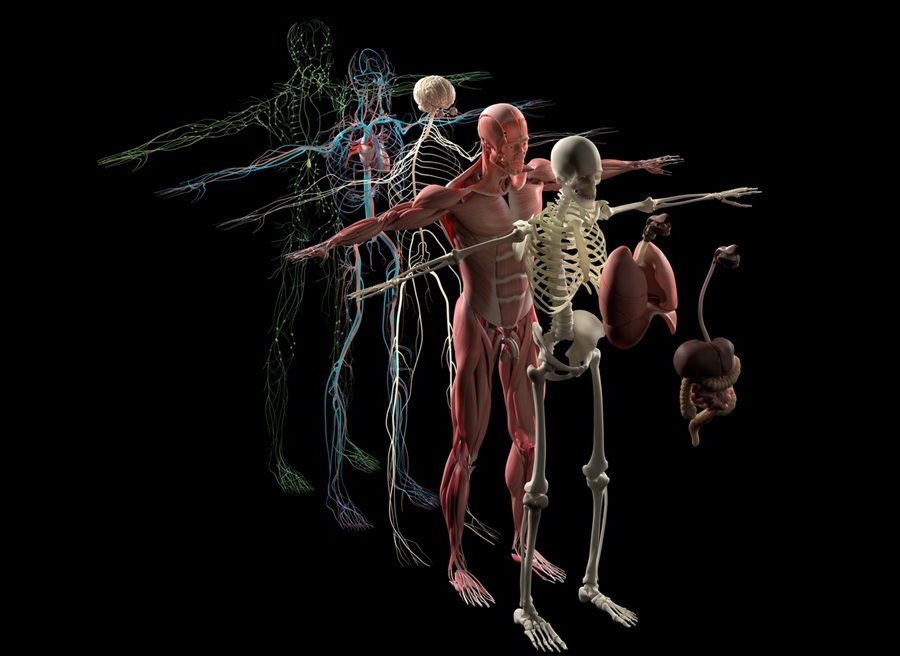
Image: A new study suggests imaging tests following primary treatment of differentiated thyroid cancer rarely leads to an improvement in chances of survival (Photo courtesy of the University of Michigan).
“Over time, we have seen this marked increase in the use of imaging after primary treatment of thyroid cancer, despite the fact that the majority of our patients have low-risk cancer. For the most part, this imaging isn't affecting survival,” concluded senior author assistant professor of medicine Megan Haymart, MD, and colleagues. “With the exception of radioiodine scans in presumed iodine avid disease, this association has shown no clear improvement in disease specific survival. These findings emphasize the importance of curbing unnecessary imaging and tailoring imaging after primary treatment to patient risk.”
Differentiated thyroid cancer has been increasing in incidence for several decades, and is expected to be the fourth leading cancer diagnosis by the year 2030; most of this rise is explained by diagnoses of small, low risk cancers, which are associated with an excellent long-term survival. Despite this, imaging tests after primary treatment of thyroid cancer is also rising, for reasons as yet unknown.
Related Links:
University of Michigan