New Imaging Tool Increases Safety of Brain Surgery
By MedImaging International staff writers
Posted on 25 Oct 2015
A new stimulated Raman scattering (SRS) microscopic technology may help surgeons differentiate between tumor and normal brain tissue in real-time.Posted on 25 Oct 2015
Under development at the University of Michigan Health System (U-M; Ann Arbor, MI, USA), New York University (NYU; NY, USA), and other institutions, the SRS microscopy technique is used to produce different signals for proteins and lipids, which can then be assigned a color—blue and green, respectively—to differentiate between brain cortex, tumor tissue, and white matter. To make the approach amenable to routine use in neuropathology, the researchers created an objective classifier that integrates image characteristics (such as protein/lipid ratio, axonal density, and degree of cellularity), into one output that can alert pathologists to tumor infiltration.
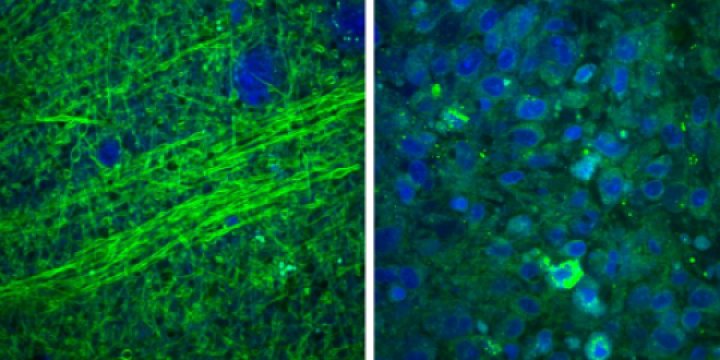
Image: Normal brain containing axons (left) under SRS microscopy, compared to disordered brain tumor tissue (right) (Photo courtesy of U-M).
The classifier was built using more than 1,400 images from patients with glioblastoma and epilepsy, and can distinguish between tumor-infiltrated and non-tumor regions with over 99% accuracy, regardless of tumor grade or histologic subtype. A subsequent study of biopsies taken from adult and pediatric patients with glioblastoma revealed not only distinctive features with SRS microscopy, but also the presence of infiltrating cells in tissues that appeared otherwise normal when examined with traditional staining techniques. The study was published on October 14, 2015, in Science Translational Medicine.
“SRS imaging technology could be used to complement existing neurosurgical workflows, allowing for rapid and objective characterization of brain tissues and, in turn, clinical decision-making,” concluded lead author neurosurgeon Daniel Orringer, MD, of U-M, and colleagues. “It allows the surgical decision-making process to become data driven instead of relying on the surgeon's best guess. We're able to visualize tumor that otherwise would be invisible to the surgeon in the operating room.”
“This technology has the potential to resolve a long-standing issue in cancer surgery, which is the need for faster and more effective methods to assess whether a tumor has been fully removed,” added Richard Conroy, PhD, of the US National Institutes of Health (NIH; Bethesda, MD, USA), which provided funding for the development of the technology. “The ability to determine tumor margins without having to send samples to a pathologist could increase patient safety and improve outcomes by shortening the length of surgeries and reducing the number of cases where cancer cells are left behind.”
Related Links:
University of Michigan Health System
New York University
US National Institutes of Health