NIR Fluorescence Imaging Technique Helps Physicians Ease the After Effects of Breast Cancer
By MedImaging International staff writers
Posted on 01 Sep 2010
A new study of breast cancer survivors may help physicians relieve a common side effect of cancer treatments. Posted on 01 Sep 2010
The collaborative research by Eva Sevick, Ph.D., director of the Center for Molecular Imaging at the University of Texas Health Science Center (UTHSC; Houston, TX, USA), and Caroline Fife, M.D., director of the Memorial Herman Wound Care Clinic at UTHSC, could bring relief to millions. Their study's findings were published in August 2, 2010, in the inaugural issue of the journal Biomedical Optics Express, an online, open-access journal published by the Optical Society (OSA; Washington DC, USA).
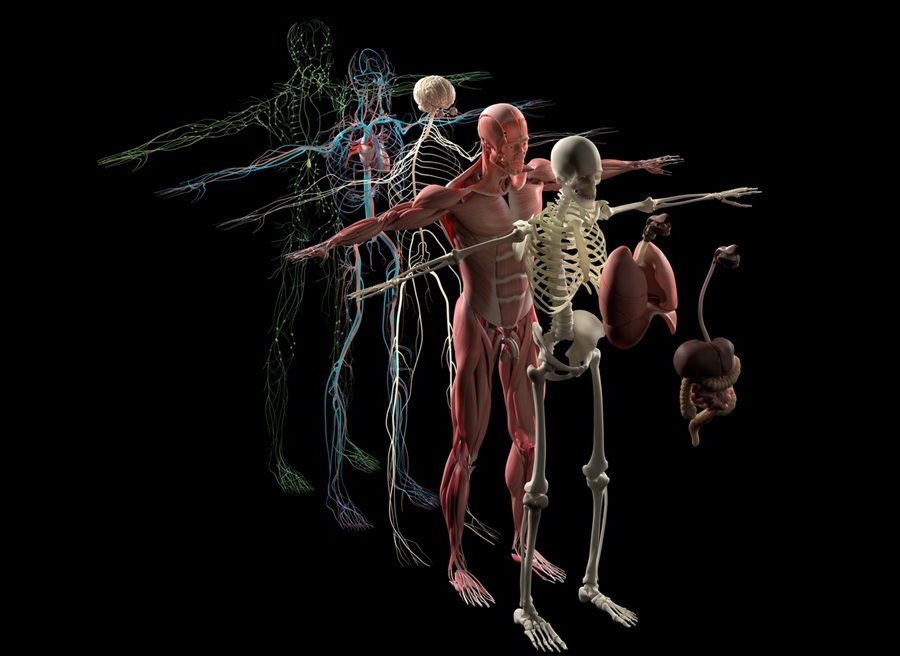
A considerable number of breast cancer survivors suffer from lymphedema in the aftermath of their cancer surgeries. In lymphedema, fluids accumulate in the arms, potentially causing disfiguring and debilitating swelling that can affect quality of life.
Treatments vary, but they typically consist of using manual and pneumatic therapies to trigger or stimulate the body to remove excess fluid and reduce tissue swelling. Finding out whether a treatment is working can take months. That is because the current method of assessing progress is to measure the circumference or volume of a limb and check for changes in swelling--and a size change big enough to be measured takes time. During this time, the condition might improve--or it might worsen.
The UTHSC researchers have developed what has the potential to be a more sensitive and instantaneous way to monitor the effectiveness of a treatment. Their new near-infrared (NIR) fluorescence imaging technique examines the root cause of lymphedema: blockages or damages in the lymphatic system that prevent fluid from circulating through the body and cause it to pool in the limbs.
Nine women--six with lymphedema and three controls--were injected with a NIR fluorescent dye that has been used safely for 50 years at much higher dosages. The dye is taken up by the lymphatic system. When tissue surfaces are exposed to a dim, near-infrared laser--harmless to the human body--the dye within fluoresces, revealing its transit through the lymphatic system. "This is the only method that can directly check for improvements in lymphatic function in one sitting, before and after a treatment," noted Dr. Sevick.
Physicians have several treatment options for controlling lymphedema. They may use compression bandages and massage limbs to encourage fluids to drain from the arm. Pneumatic compression devices, sleeves made of segmented chambers that inflate and squeeze, may provide a comparable benefit at home. "The problem is that there has been no good way to measure direct evidence of benefit," stated Dr. Sevick. "Hopefully we can use near-infrared fluorescence imaging technique to show improved lymphatic function from these treatments."
The NIR fluorescence technique detected statistically significant improvements in fluid flow through the lymphatic system immediately after the use of pneumatic compression devices. A larger follow-up study will be needed to validate the results of this pilot study, says Sevick.
The research was funded by the U.S. National Institutes of Health (Bethesda, MD, USA) and by Tactile Systems Technology, Inc. (Minneapolis, MN, USA), which manufactures and markets the Flexitouch pneumatic compression devices tested in this research.
Related Links:
University of Texas Health Science Center
Tactile Systems Technology










 Guided Devices.jpg)