3D MRI Offers Improved Prediction of Survival After Chemotherapy for Liver Tumors
|
By MedImaging International staff writers Posted on 17 Apr 2014 |
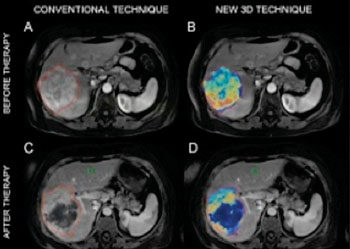
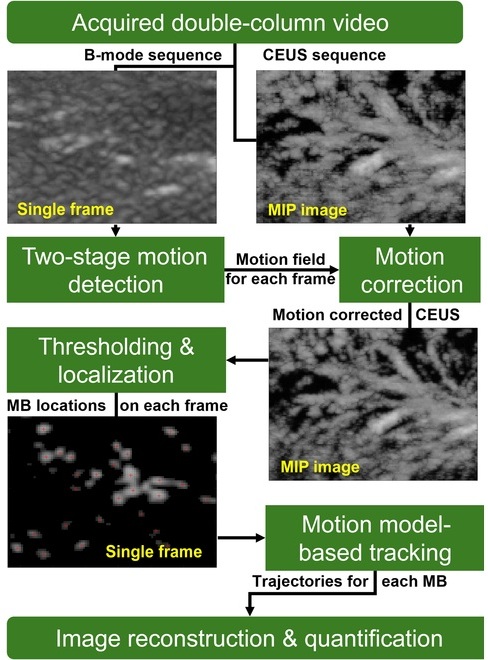
Image: The quantitative character of the novel 3D technique on MR scans from a patient with primary liver cancer is demonstrated. Images A and B show the scan of the patient before being treated with chemoembolization. The new 3D technique helped quantify the volume and distribution of viable tumor tissue (shown in red and yellow colors). Images C and D demonstrate MR scans acquired after the treatment. The new 3D method helped the radiologists to quantify the vast central destruction of the tumor after the treatment (the dead tumor is represented by the blue color) (Photo courtesy of Johns Hopkins Medicine).
Researchers are using specialized three-dimensional (3D) magnetic resonance imaging (MRI) scanning technology to accurately measure living and dying liver tumor tissue in order to quickly show whether very toxic chemotherapy, delivered right through a tumor’s blood supply, is working.
The Johns Hopkins University (Baltimore, MD, USA) investigators noted that their findings, presented on March 22–27, 2014, in San Diego (CA, USA), at the annual meeting of the Society of Interventional Radiology, are the first “proof of principle” that this technology can show tumors in three dimensions and effectively measure tumor viability and death. Early data of a series of studies involving 140 US men and women with liver tumors were also presented at the Radiological Society of North America (RSNA) annual meeting, December 1–6, 2013, in Chicago (IL, USA).
The researchers also reported that their findings in patients with either primary liver cancers or metastatic tumors from cancers beginning in other areas of the body are evidence that using this technology before and after treatment is a faster and better tool for predicting patient survival after chemotherapy targeted directly at tumors, called chemoembolization.
Unlike standard methods to assess tumor response after chemoembolization, which are based on two-dimensional images and tumor size, the Johns Hopkins-developed 3D technology also distinguishes between dead and live tissue, giving an accurate evaluation of tumor cell death.
The new technology builds on conventional 2D techniques and uses computer analytics to evaluate the amount of so-called contrast dye absorbed by tumor tissue. The dye is injected into patients before their MRI scan to enhance image production. Researchers say live tissue will absorb more dye than dead tissue, affecting image brightness, which can also be measured for size and intensity. "Our high-precision, 3D images of tumors provide better information to patients about whether chemoembolization has started to kill their tumors so that physicians can make more well-informed treatment recommendations,” stated Johns Hopkins interventional radiologist Jean-Francois Geschwind, MD, senior investigator on the studies.
Dr. Geschwind, a professor in the department of radiology at the Johns Hopkins University School of Medicine and its Kimmel Cancer Center, stated that determining the real degree of a tumor’s response to chemoembolization is especially important for patients with moderate to advanced stages of the disease, whose liver tumors might at first be too large or too many to surgically remove.
In the first study, researchers compared the conventional imaging technology and the newly developed technology in 17 Baltimore men and women with advanced liver cancer. All were treated with surgery or liver transplantation after chemoembolization. The research team used existing MR analysis techniques, as well as the new 3D technology to compare the radiologists’ studies with pathologic review of tumor samples after therapy and surgical removal. The error margin of the new 3D image analysis, they reported, was low (at up to 10%) when predicting the amount of dead tumor tissue found by pathologists whereas the standard, 2D method deviated by as much as 40% from actual values.
Dr. Geschwind and his colleagues, in further studies, used the conventional and new imaging techniques to study the MRI scans of more than 300 liver tumors in some 123 other men and women, also from the Baltimore region. All patients were treated at The Johns Hopkins Hospital between 2003 and 2012, and each received pre- and post-chemoembolization MRI scans to assess the effects of therapy on the tumors.
Using the new 3D technique, Dr. Geschwind’s team discovered that patients who responded well to therapy lived 19 months longer (a median of 42 months) than patients who did not respond well (average 23 month survival). Standard techniques revealed slightly less disparity in survival (average 18 months longer) between patients who responded to therapy and those who did not respond.
Dr. Geschwind reported that the 3D technology’s improved accuracy removes a lot of the guesswork that now goes into evaluating treatment outcomes. The new assessment takes seconds to perform, he added, so radiologists can provide faster, nearly instantaneous treatment guidance. The investigators plan additional software modifications to the new application before training more physicians to use it. He also has plans to study how it can affect treatment decisions, and whether these therapy choices help individuals lead a longer life.
The software used in the MRI scans was developed at Johns Hopkins and at Philips Research North America (Briarcliff Manor, NY, USA). Philips Healthcare, whose parent company is based in the Netherlands, manufactures some of the MRI scanners used in the study.
Related Links:
Johns Hopkins University
Philips Research North America
The Johns Hopkins University (Baltimore, MD, USA) investigators noted that their findings, presented on March 22–27, 2014, in San Diego (CA, USA), at the annual meeting of the Society of Interventional Radiology, are the first “proof of principle” that this technology can show tumors in three dimensions and effectively measure tumor viability and death. Early data of a series of studies involving 140 US men and women with liver tumors were also presented at the Radiological Society of North America (RSNA) annual meeting, December 1–6, 2013, in Chicago (IL, USA).
The researchers also reported that their findings in patients with either primary liver cancers or metastatic tumors from cancers beginning in other areas of the body are evidence that using this technology before and after treatment is a faster and better tool for predicting patient survival after chemotherapy targeted directly at tumors, called chemoembolization.
Unlike standard methods to assess tumor response after chemoembolization, which are based on two-dimensional images and tumor size, the Johns Hopkins-developed 3D technology also distinguishes between dead and live tissue, giving an accurate evaluation of tumor cell death.
The new technology builds on conventional 2D techniques and uses computer analytics to evaluate the amount of so-called contrast dye absorbed by tumor tissue. The dye is injected into patients before their MRI scan to enhance image production. Researchers say live tissue will absorb more dye than dead tissue, affecting image brightness, which can also be measured for size and intensity. "Our high-precision, 3D images of tumors provide better information to patients about whether chemoembolization has started to kill their tumors so that physicians can make more well-informed treatment recommendations,” stated Johns Hopkins interventional radiologist Jean-Francois Geschwind, MD, senior investigator on the studies.
Dr. Geschwind, a professor in the department of radiology at the Johns Hopkins University School of Medicine and its Kimmel Cancer Center, stated that determining the real degree of a tumor’s response to chemoembolization is especially important for patients with moderate to advanced stages of the disease, whose liver tumors might at first be too large or too many to surgically remove.
In the first study, researchers compared the conventional imaging technology and the newly developed technology in 17 Baltimore men and women with advanced liver cancer. All were treated with surgery or liver transplantation after chemoembolization. The research team used existing MR analysis techniques, as well as the new 3D technology to compare the radiologists’ studies with pathologic review of tumor samples after therapy and surgical removal. The error margin of the new 3D image analysis, they reported, was low (at up to 10%) when predicting the amount of dead tumor tissue found by pathologists whereas the standard, 2D method deviated by as much as 40% from actual values.
Dr. Geschwind and his colleagues, in further studies, used the conventional and new imaging techniques to study the MRI scans of more than 300 liver tumors in some 123 other men and women, also from the Baltimore region. All patients were treated at The Johns Hopkins Hospital between 2003 and 2012, and each received pre- and post-chemoembolization MRI scans to assess the effects of therapy on the tumors.
Using the new 3D technique, Dr. Geschwind’s team discovered that patients who responded well to therapy lived 19 months longer (a median of 42 months) than patients who did not respond well (average 23 month survival). Standard techniques revealed slightly less disparity in survival (average 18 months longer) between patients who responded to therapy and those who did not respond.
Dr. Geschwind reported that the 3D technology’s improved accuracy removes a lot of the guesswork that now goes into evaluating treatment outcomes. The new assessment takes seconds to perform, he added, so radiologists can provide faster, nearly instantaneous treatment guidance. The investigators plan additional software modifications to the new application before training more physicians to use it. He also has plans to study how it can affect treatment decisions, and whether these therapy choices help individuals lead a longer life.
The software used in the MRI scans was developed at Johns Hopkins and at Philips Research North America (Briarcliff Manor, NY, USA). Philips Healthcare, whose parent company is based in the Netherlands, manufactures some of the MRI scanners used in the study.
Related Links:
Johns Hopkins University
Philips Research North America
Latest MRI News
- Cutting-Edge MRI Technology to Revolutionize Diagnosis of Common Heart Problem
- New MRI Technique Reveals True Heart Age to Prevent Attacks and Strokes
- AI Tool Predicts Relapse of Pediatric Brain Cancer from Brain MRI Scans
- AI Tool Tracks Effectiveness of Multiple Sclerosis Treatments Using Brain MRI Scans
- Ultra-Powerful MRI Scans Enable Life-Changing Surgery in Treatment-Resistant Epileptic Patients
- AI-Powered MRI Technology Improves Parkinson’s Diagnoses
- Biparametric MRI Combined with AI Enhances Detection of Clinically Significant Prostate Cancer
- First-Of-Its-Kind AI-Driven Brain Imaging Platform to Better Guide Stroke Treatment Options
- New Model Improves Comparison of MRIs Taken at Different Institutions
- Groundbreaking New Scanner Sees 'Previously Undetectable' Cancer Spread
- First-Of-Its-Kind Tool Analyzes MRI Scans to Measure Brain Aging
- AI-Enhanced MRI Images Make Cancerous Breast Tissue Glow
- AI Model Automatically Segments MRI Images
- New Research Supports Routine Brain MRI Screening in Asymptomatic Late-Stage Breast Cancer Patients
- Revolutionary Portable Device Performs Rapid MRI-Based Stroke Imaging at Patient's Bedside
- AI Predicts After-Effects of Brain Tumor Surgery from MRI Scans
Channels
Radiography
view channel
AI Improves Early Detection of Interval Breast Cancers
Interval breast cancers, which occur between routine screenings, are easier to treat when detected earlier. Early detection can reduce the need for aggressive treatments and improve the chances of better outcomes.... Read more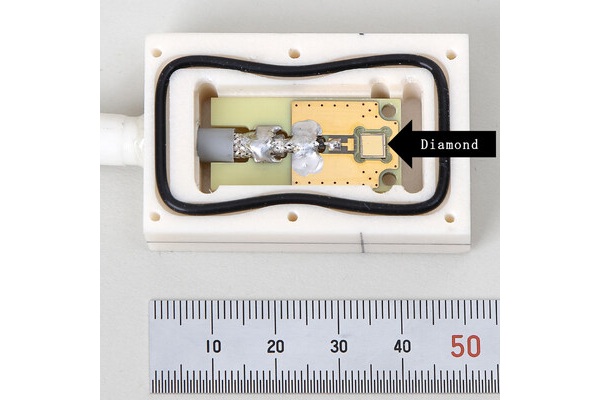
World's Largest Class Single Crystal Diamond Radiation Detector Opens New Possibilities for Diagnostic Imaging
Diamonds possess ideal physical properties for radiation detection, such as exceptional thermal and chemical stability along with a quick response time. Made of carbon with an atomic number of six, diamonds... Read moreUltrasound
view channel.jpeg)
AI-Powered Lung Ultrasound Outperforms Human Experts in Tuberculosis Diagnosis
Despite global declines in tuberculosis (TB) rates in previous years, the incidence of TB rose by 4.6% from 2020 to 2023. Early screening and rapid diagnosis are essential elements of the World Health... Read more
AI Identifies Heart Valve Disease from Common Imaging Test
Tricuspid regurgitation is a condition where the heart's tricuspid valve does not close completely during contraction, leading to backward blood flow, which can result in heart failure. A new artificial... Read moreNuclear Medicine
view channel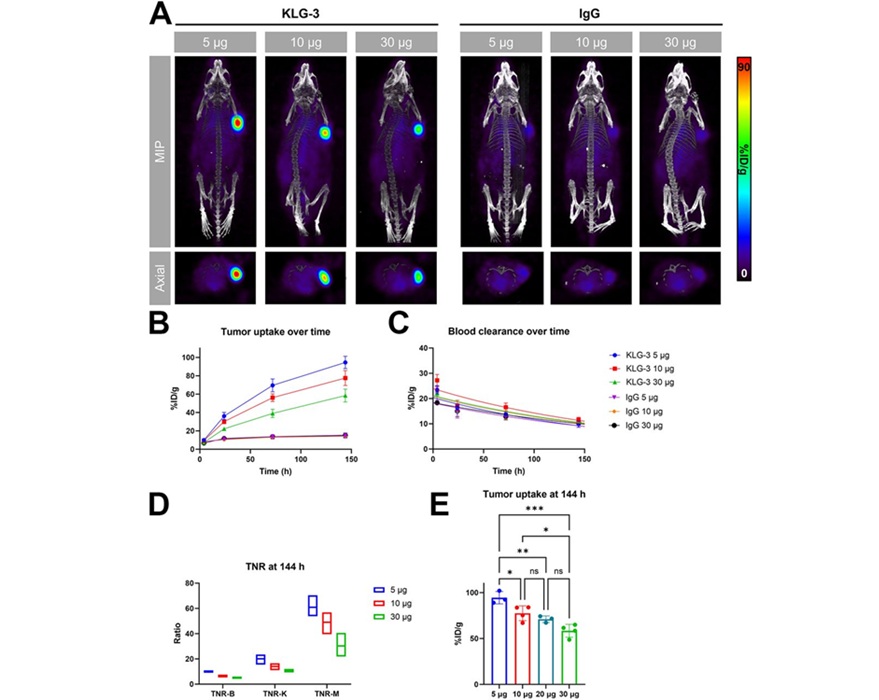
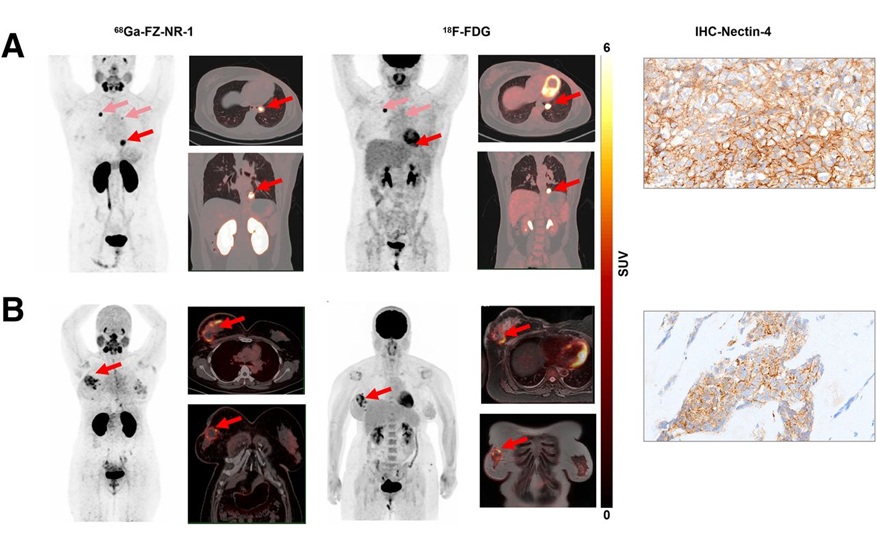
Novel Radiolabeled Antibody Improves Diagnosis and Treatment of Solid Tumors
Interleukin-13 receptor α-2 (IL13Rα2) is a cell surface receptor commonly found in solid tumors such as glioblastoma, melanoma, and breast cancer. It is minimally expressed in normal tissues, making it... Read more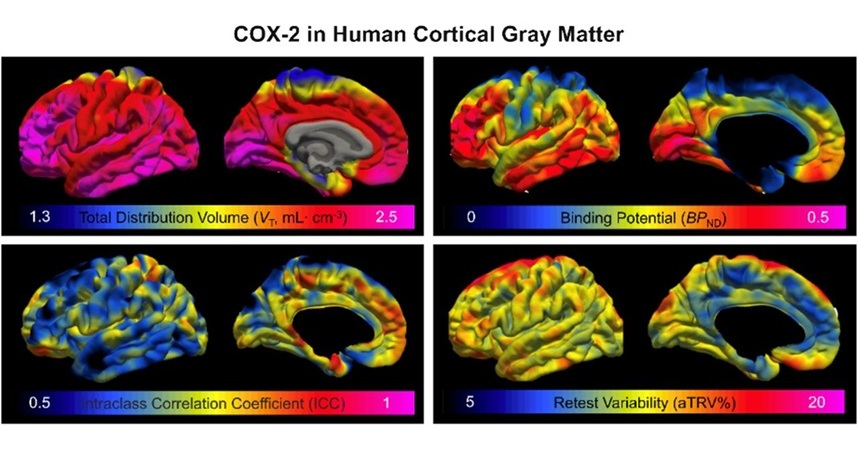
Novel PET Imaging Approach Offers Never-Before-Seen View of Neuroinflammation
COX-2, an enzyme that plays a key role in brain inflammation, can be significantly upregulated by inflammatory stimuli and neuroexcitation. Researchers suggest that COX-2 density in the brain could serve... Read moreGeneral/Advanced Imaging
view channel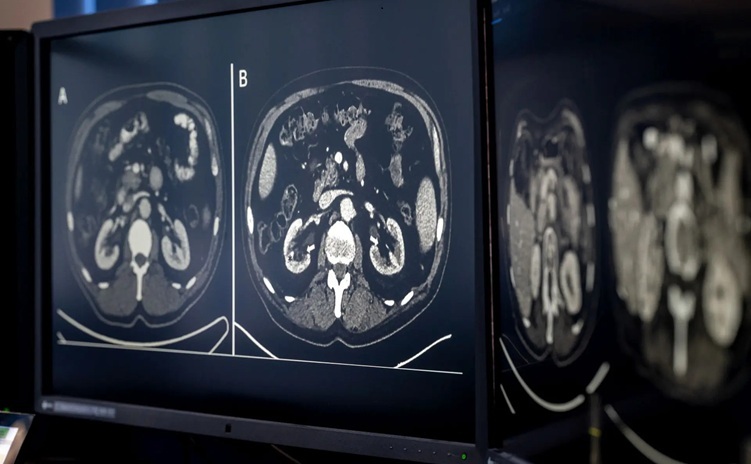
AI-Based CT Scan Analysis Predicts Early-Stage Kidney Damage Due to Cancer Treatments
Radioligand therapy, a form of targeted nuclear medicine, has recently gained attention for its potential in treating specific types of tumors. However, one of the potential side effects of this therapy... Read more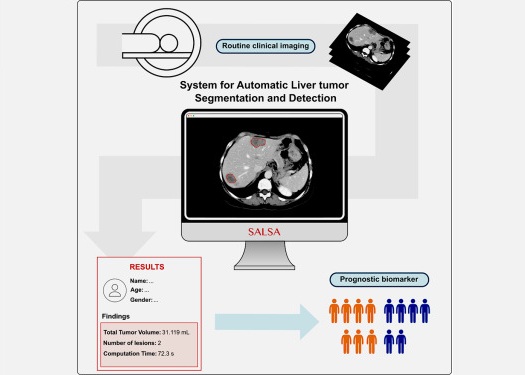
CT-Based Deep Learning-Driven Tool to Enhance Liver Cancer Diagnosis
Medical imaging, such as computed tomography (CT) scans, plays a crucial role in oncology, offering essential data for cancer detection, treatment planning, and monitoring of response to therapies.... Read moreImaging IT
view channel
New Google Cloud Medical Imaging Suite Makes Imaging Healthcare Data More Accessible
Medical imaging is a critical tool used to diagnose patients, and there are billions of medical images scanned globally each year. Imaging data accounts for about 90% of all healthcare data1 and, until... Read more
Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
The global artificial intelligence (AI) in medical diagnostics market is expanding with early disease detection being one of its key applications and image recognition becoming a compelling consumer proposition... Read moreIndustry News
view channel
GE HealthCare and NVIDIA Collaboration to Reimagine Diagnostic Imaging
GE HealthCare (Chicago, IL, USA) has entered into a collaboration with NVIDIA (Santa Clara, CA, USA), expanding the existing relationship between the two companies to focus on pioneering innovation in... Read more
Patient-Specific 3D-Printed Phantoms Transform CT Imaging
New research has highlighted how anatomically precise, patient-specific 3D-printed phantoms are proving to be scalable, cost-effective, and efficient tools in the development of new CT scan algorithms... Read more
Siemens and Sectra Collaborate on Enhancing Radiology Workflows
Siemens Healthineers (Forchheim, Germany) and Sectra (Linköping, Sweden) have entered into a collaboration aimed at enhancing radiologists' diagnostic capabilities and, in turn, improving patient care... Read more




 Guided Devices.jpg)